When a person's kidneys fail to function properly, life-sustaining treatment, such as hemodialysis, may be required. Hemodialysis works by removing blood from the body; putting it through a dialyzer to clean the blood of toxins, excess water, and electrolytes; and then returning clean blood back to the patient (see Picturing hemodialysis). There are approximately 300,000 people receiving hemodialysis three times a week. At this rate, it's likely that you'll prepare a patient for hemodialysis. In this article, you'll learn what you need to do minimally to keep your patient safe before and after a hemodialysis treatment.
The nuts and bolts of hemodialysis
Hemodialysis can be performed using one of three different access devices. The most common access used is an arteriovenous fistula (AVF), which is created peripherally by connecting an artery and vein together. This surgical connection of the artery and vein causes increased blood flow, which stimulates the size and thickness of the AVF. After about 6 to 12 weeks, the AVF is strong enough to withstand the high volumes of blood flow needed for dialysis treatments.
When a patient doesn't have blood vessels strong enough to grow adequately, an arteriovenous graft(AVG) may be created. An AVG is created by using synthetic material to connect the artery to a vein. The time required for an AVG to mature in size is usually about 3 weeks. Whether your patient has an AVF or an AVG, time is needed for it to grow (see AVF and AVG access). Meanwhile, a temporaryhemodialysis catheter will be placed in your patient's subclavian, femoral, or internal jugular vein for immediate use (see Hemodialysis catheter access). Regardless of the type of access device your patient has, there are precautions you'll need to take before you send your patient for a dialysis treatment.
Patients on dialysis are typically on a 3 days a week schedule. Treatment usually lasts for 3 to 5 hours. What you do before your patient has dialysis can make all the difference in how well your patient responds to the treatment. In some rare cases, what you do or don't do can even make the difference between life and death. This is why it's very important to make sure you understand what should and should never occur when preparing your patient for hemodialysis.
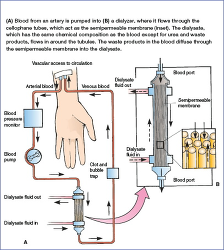 | Figure. Picturing hemodialysis |
Before hemodialysis
Weight
Before your patient undergoes a hemodialysis treatment, you'll need to obtain an accurate weight measurement. Expect that your patient will be a few pounds heavier than the previous day; this is the result of water buildup between treatments. Document the weight obtained and be sure to share this with the hemodialysis nurse. The weight measurement will help determine the amount of fluid that will need to be removed during hemodialysis so that your patient can return to his dry weight. The dry weight is the patient's goal weight without the fluid buildup between hemodialysis treatments.
Vital signs
Obtain a complete set of vital signs and document your findings. Assess whether your patient's BP indicates hypertension or hypotension. Avoid monitoring BP in the arm with the AVF or AVG; doing so can cause clotting and result in loss of access. Assess your patient's temperature for fever, which could indicate infection. Assess the rate and quality of respirations. Patients undergoing hemodialysis are prone to the development of dysrhythmias; when assessing the heart rate, be sure to also take note of the rhythm.
During the time you collect vital signs, it's also a good time to assess the overall condition of your patient. Do this by assessing his skin, mental status, and whether your patient has any complaints, such as pain or nausea.
Access site
Before sending your patient for a hemodialysis treatment, you'll need to make sure that the access site is functioning properly. Your assessment interventions will depend on the type of access your patient has. If your patient has an AVF or AVG, you'll need to check for obvious problems. Assess for bleeding at the site, oozing or drainage, redness, warmth, and patient complaints of pain at the site because these are key signs of infection and should be reported to the healthcare provider.
It's extremely important to assess the site for circulation. This is done by assessing distal pulses, palpating for a thrill (feel the thrill), and auscultating for a bruit (hear the buzz). You will feel the thrill by gently placing your fingertips or palm over your patient's access site; you should notice a vibration. To hear the bruit, place your stethoscope over the site and listen for a swishing or whooshing sound. If either is absent or barely noticeable, it could indicate loss of access and you'll need to contact the healthcare provider in addition to the hemodialysis nurse for instructions on how to proceed before sending your patient for treatment.
When dialysis is anticipated on a short-term basis or during the period of time when an AVF or AVG matures, your patient may have a hemodialysis catheter placed. These catheters are most often placed in the subclavian vein, but can also be placed in the internal jugular or femoral veins. A hemodialysis catheter has two lumens: one will be used to remove blood and the other to return the clean blood back to the patient. When assessing this type of access, you'll need to monitor the catheter site for drainage and redness of surrounding skin. It's very important that you maintain sterile technique when working with hemodialysis catheters. You shouldn't use these catheters to administer routine fluids or medications, and they shouldn't be flushed with normal saline solution. Most facilities restrict use of these catheters to only the hemodialysis nurse; review your facility's policy on your responsibilities when caring for a hemodialysis catheter.
Lab results
Review the last ordered lab results; specifically review the chemistry results for levels of sodium, potassium, phosphorus, blood urea nitrogen, and creatinine. Anticipate that these will be elevated. Knowing the predialysis electrolyte results will help determine the effectiveness of the treatment by comparing them with the postdialysis lab results.
Review the complete blood cell count, particularly the red blood cell (RBC) count, hemoglobin, and hematocrit levels. Anticipate that these will be decreased from normal levels, but understand that dialysis doesn't correct abnormal RBC, hemoglobin, and hematocrit levels. You should anticipate receiving other orders to address these low levels; for example, administration of packed RBCs and RBC-stimulating medication (also known as erythropoiesis-stimulating agents).
Important reminder: Make sure that labs are never drawn from the arm with the AVF or AVG.
Scheduled medications
Review the list of medications for your patient, scheduled up to 4 hours before the treatment. There may be some that you shouldn't administer. Because your patient's BP will drop during treatments, all antihypertensive drugs should be held before hemodialysis. In most cases, antiarrhythmic medications are given as scheduled due to the high incidence of patients developing arrhythmias during hemodialysis. Certain types of drugs will pass through the dialysis machine and not provide benefits to the patient. These drugs are any type of water-soluble vitamins, so they should also be held before treatments.
Your facility will provide guidelines for the safe administration of medications to patients before and after hemodialysis treatments. Remember to contact the healthcare provider for individualized orders for your patient.
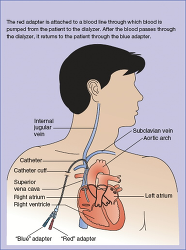 | Figure. Hemodialysis catheter access |
After hemodialysis
Your nursing interventions when your patient returns from a hemodialysis treatment are almost identical to your predialysis interventions. As soon as you resume care of your patient postdialysis, you'll need to obtain a set of vital signs and a weight measurement and assess the access site. Compare your findings with the predialysis results and report anything not within the defined limits as predetermined by the healthcare provider. Infection is a complication that should be continually assessed by looking for elevations in temperature and white blood cell count and assessing for warmth and redness at or around the access site. Monitor the access site carefully for bleeding. Early detection and treatment can prevent life-threatening hemorrhaging that could result from heparin used during treatments. Monitor your patient closely for signs of confusion, decreased level of consciousness, and sudden severe headaches because these neurologic changes could be related to a potentially life-threatening complication known as disequilibrium syndrome and must be reported immediately.
Determine when the next ordered labs will be collected and keep a lookout for the results to review. You'll also need to give the medications that were held before sending your patient to hemodialysis. This should be done only after your patient has stabilized, which is usually within 2 to 4 hours after treatment.
Live long and prosper
The number of people requiring dialysis is increasing every year. Patients with kidney failure can live long and productive lives with the help of hemodialysis. Nurses who practice in acute care hospitals, dialysis clinics, and even home health may be responsible for providing direct care to a patient in need of hemodialysis. This article describes the minimal interventions that must be done each time you send and receive a patient to and from a hemodialysis treatment. Using this information, in addition to the specific policies and guidelines at your facility, will help to ensure you provide the best possible care to your patient.

No comments:
Post a Comment